Workplace shielding and doctors at higher risk of harm working in anaesthesia and critical care during the COVID-19 pandemic
16 July 2020
Summary
Employers have a legal responsibility to provide a safe environment for employees.
Shielding doctors and doctors at higher risk have a responsibility to mitigate risks to themselves if they plan to return to work. This will involve assessment of personal risk, modification of this where possible and full engagement with risk mitigation when at work and travelling to and from work.
Assessments regarding individual risk may be undertaken at a departmental or divisional level. Consideration should be given to options including delayed return, remote working, redeployment or rearrangement of working patterns and location to mitigate risk. Occupational Health, and where necessary Human Resources, departments should have oversight of processes, and involvement when decisions are complex.
Departments of anaesthesia and critical care medicine should provide a safe environment for returning shielding doctors and doctors at higher risk; a departmental risk assessment should be undertaken to ensure that appropriate mitigation measures are in place. This will include risk mitigation policies and practices.
Individuals in departments should all adhere to those working practices designed to reduce transmission of SARS-CoV-2 between staff and others.
Necessary adjustments to work pattern, environment and processes should be agreed between the employee’s line manager and the employee, where necessary in consultation with Occupational Health and Human Resources, before their return to work.
For those returning to work, there will be a transition period that will require support structures that should be tailored to the individual and departmental needs.
Trainees should receive specific support from their Training Programme Directors and School of Anaesthesia to enable completion of missed components of training. When more prolonged absence of work is necessary, postgraduate medical training bodies may also be involved in reaching mutually satisfactory plans for future return to training.
When employer and employee cannot reach agreement about actions to be taken, local resolution policies, mediation and the involvement of the Local Negotiating Committee are recommended. Trade union support or involvement in negotiation may become necessary.
All these measures should be balanced against the safety and protection of those in lower risk categories, such that protection of all staff is equitable, non-discriminatory and does not interfere with the safe delivery of patient care.
The COVID-19 pandemic has been an especially challenging time for all concerned. Anaesthetists and doctors working in critical care who have been shielding will have had notably different experiences from those involved in direct patient care. It is important to acknowledge all individual contributions during this period and in addition to thank the families, friends, colleagues and departments who have supported the shielding workforce.
Community shielding and workplace shielding
Community shielding protects the clinically extremely vulnerable from exposure to and harm from SARS-CoV-2 infection. Relevant individuals should have been contacted directly and instructed on actions to take. Health conditions currently include patients with solid organ transplants, certain cancers, significant immune deficiency through disease or treatment, severe respiratory conditions and pregnant women with significant heart disease. The list gives latitude to clinicians to include conditions outside the designated list. Because of inherent risks posed by working in healthcare, a broader group of individuals has been shielded for their protection from increased risks in the workplace (workplace shielding). A further group is shielding to protect clinically extremely vulnerable members of their family (shielding by proxy). Finally, other doctors are at higher risk, but are not shielding because they do not meet specific criteria or have chosen not to shield. For those who are workplace shielding, there will be a two-stage assessment of when to stop shielding: first when to stop community shielding, i.e. to leave home, and secondly when or whether to stop workplace shielding, i.e. when to return to work.
Actions for individuals
This document has been written for anaesthetists and doctors working in critical care who are currently shielding. It is also written for those with a role in supporting or managing the above individuals, including Clinical Directors, College Tutors, and professionals working in Occupational Health and Human Resources. Much of this document also applies to doctors at higher risk.
A review published in Anaesthesia discusses biological and environmental risk and includes a tool to enable individual estimation of relative risk. This may inform decision-making and aid discussions with other relevant professionals.
Shielding doctors and doctors at higher risk
These doctors have a responsibility to mitigate risks to themselves when considering a return to work.
Mitigation includes:
- Liaising with department leaders, Occupational Health and Human Resources as necessary.
- Modification of personal health risk where possible:
Ensuring chronic health conditions are as well controlled as possible, especially diabetes, asthma, blood pressure and weight control. When appropriate shielding requirements should be reassessed with a clinical specialist;
Stopping smoking;
Considering psychological wellbeing and seeking support if psychological issues are a factor in relation to returning, as this may require intervention before return to work and during and transition period.
- Engaging in assessment of personal risk and acting on the outcomes, which may include:
Returning to lower risk work, returning to non-clinical work or returning to work with mitigation;
Working from home or taking prolonged leave or a sabbatical;
Rarely, a change in specialty for trainees, or retiring for older doctors;
- Full engagement in risk mitigation when at work (Box 1)
- At work, consideration of:
Avoiding higher risk patients, e.g. redeployment from critical care to anaesthesia or within anaesthesia from emergency/unshielded patients to locations dealing exclusively with swab-negative and shielded patients;
Avoiding higher risk procedures when practical, e.g. limiting direct involvement with aerosol generating procedures (AGPs);
Avoiding work patterns involving predictable or unpredictable exposure to high risk, e.g. emergency work and on call duties;
Wearing a higher level of personal protective equipment (PPE), e.g. sessional use of a non-valved FFP3 instead of a face mask in higher risk locations such as ICU or operating theatres.
- Minimising risk when travelling to and from work, e.g. avoiding public transport, mask wearing and social distancing as appropriate.
- Appropriate management of work clothes and equipment on returning home to minimise risk of household contamination.
- Considering wearing a facemask in all public settings
Employers and clinical leaders
Employers have a legal responsibility to provide a safe environment for employees. Departments of anaesthesia and critical care medicine have a role to play in supporting this responsibility. The Health and Safety Executive (HSE) outline an employer’s legal responsibility during the COVID-19 outbreak stating that “reasonable steps to protect your workers and others from coronavirus” must be made. They emphasise risk assessments, protecting people at higher risk and making the workplace “COVID-secure”. This responsibility extends to returning shielding doctors and doctors at higher risk, and specific advice on fitness to work and discussion of reasonable adjustments. NHS Employers recommends and provides guidance on risk assessments for staff and a list of potential outputs. There are numerous risk tools available: that referred to by NHS employers, from the Faculty of Occupational Heath, emphasises a wide assessment of workplace and workforce but lacks individualised quantitative outputs. Other risk tools are signposted in the resources section, and a risk assessment tool kit is the accompanying document.
Assessments regarding individual risk may be undertaken at a departmental or divisional level. Occupational Health, and where necessary Human Resources, departments should have oversight of processes and involvement when decisions are complex. The aim should be achieving a mutually satisfactory response to changing circumstances. Consideration should be given to all options listed above, although the list is not exclusive.
If the risk of environmental exposure increases in the future, it may be necessary for doctors who are at higher risk to consider shielding again, and planning for this should from part of a risk assessment.
All the above measures should be balanced against the safety and protection of those in lower risk categories, such that protection of all staff is equitable, non-discriminatory and does not interfere with safe delivery of patient care.
Mitigation of risk by organisations includes:
Undertaking individual risk assessments and taking appropriate actions in response to the findings;
Monitoring for local community outbreaks. Increases in community activity may be indicated by national, regional or local increases in prevalence or by a reproduction number (R0) >1;
Monitoring for in-hospital environmental risk. High or increasing in-hospital risk can only be determined by testing patients and staff to monitor infection rates (antigen testing via throat/nose swabs) and seropositivity rates (antibody testing blood tests);
Reassessing individual risk when monitoring indicates an increased environmental (community or hospital) risk, as this will disproportionately affect staff who are at high risk of harm;
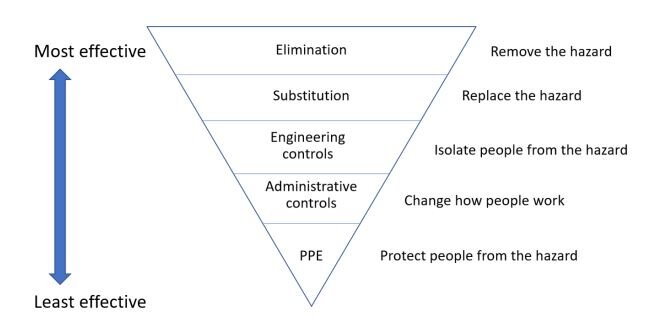
Establishing, implementing and maintaining standard infection control precautions and transmission-based precautions. The occupational health hierarchy of controls should be applied (Figure 1 and Box 1)
Maintaining segregation of patients by level of risk; e.g.
COVID-19 positive (antigen positive or diagnosed on basis of clinical diagnosis);
Untested suspected or emergency patient;
Antigen negative but unshielded;
Antigen negative and shielded.
Figure 1
|
Mitigation measures |
Box 1
Employers should also pay attention to employee wellbeing. This includes provision of readily accessible psychological and practical support, provision of appropriate rest areas where social distancing can be practised and encouraging peer support.
Clinical Directors and College Tutors
A departmental risk assessment should be undertaken to ensure appropriate measures have been taken to provide a safe environment for all staff including returning shielding doctors and doctors at higher risk. The department should be adaptable and flexible to enable shielding doctors to return to new or modified roles. Akin to the way some departments manage job plans to accommodate the needs of the ageing doctor, departments will need to adjust to incorporate safe roles for staff who are at increased risk. Actions should be fair and avoid discrimination or disadvantage to doctors at lower risk. Departmental leaders should act to ensure all staff adhere to national and local policies. Doctors at higher risk should be supported if it becomes necessary to ask colleagues to respect social distancing or implement measures described above.
Departmental and other hospital staff
Staff infection within hospitals is a significant cause for concern. All staff members should follow nationally and locally implemented measures designed to reduce transmission of infection to patients and staff, including staff members at higher risk. This is particularly important when environmental risk is high or increasing. Measures include but are not limited to those listed in Box 1. Of particular importance are understanding and adhering to policies and guidelines relating to standard infection control and transmission-based precautions, meticulous hand hygiene and use of appropriate PPE. It is important to emphasise that mitigation measures apply to staff-only areas in addition to clinical areas.
Considerations for Trainees
Trainees may have particular concerns. They will often have been employed in a department for only a short period of time and will be less well established than permanent staff. Professional hierarchy may impact on their ability or desire to discuss their personal circumstances with seniors. Time away from work has an impact on specific components of training that may be very difficult to replace. Trainees are therefore more likely to fear stigma from shielding and to have significant worries about training and career progression.
Specific support led by College Tutors, Training Programme Directors, postgraduate training bodies, Health Education England (HEE) and equivalent bodies in the devolved nations is needed to enable remote learning and when feasible gaining of competencies and adjusted progression of training.
For those returning after a relatively short period of shielding, the HEE website provides a resource for trainees about adaptations to training due to COVID-19, and emphasises the need to catch up competencies “in the next year”. This arguably creates a necessity for accelerated training for trainees and increases the workload for trainees and trainers. The Scotland deanery has published specific guidance on shielding (see resources). E-learning for health has a package on supported return to training. The RCoA and FICM have published guidance for examination candidates, including extending some examination eligibility periods.
When more prolonged absence of work is necessary, those postgraduate training bodies will need to work with shielding trainees to support trainees’ education and to reach mutually satisfactory plans for future return to training. Health Education England provides advice on supporting return to training on its SupporRTT website, which has a specific COVID-19 related section. Trainees should follow this framework to ensure a planned and fully supervised return to training. The Academy of Medical Royal Colleges has produced updated guidance for doctors in training who wish to change specialties. The ‘Gold guide’ from the Conference of Postgraduate Medical Deans (COPMeD) indicates as of March 2020 that continuous absence from training for two years should trigger a review of maintenance or withdrawal of the contract.
Of note, an increase in critical care medicine training numbers in all home countries has already occurred. It is likely that changes in healthcare priorities may necessitate further increases in numbers of anaesthetists and intensivists. Both factors make addressing the needs of shielding trainees an immediate and longer-term priority, as we can ill afford to lose these doctors from the workforce.
Reaching agreements
The employer, the doctor’s line manager and the shielding doctor should work together to undertake a risk assessment and formulate a plan. The agreed outcome of this assessment should be documented. For trainees, College Tutors will also play a key role.
When the agreement is that the doctor shall return to work, documentation should usefully include agreed adjustments to working pattern, environment and processes before any return to work.
Some risk assessments will be complex. A lack of an agreed risk assessment tool and the dynamic situation (emerging knowledge about a new disease, continuing uncertainty and risk that is changing over time) hamper objective assessment.
In most cases, the decision as to whether to continue shielding will be made by the doctor after risk 7 assessment and personal reflection. Risk assessments may be complex when doctors are shielding by proxy and in two-doctor families. It is logical that all doctors in this position are offered individual risk assessment. Where the outcome of a risk assessment is not a permanent outcome, further review should be scheduled. In most circumstances the risk assessment and reflection will lead to an agreement on outcome. When agreements cannot be reached during decision making, employer’s written processes on how to resolve disputes should be followed. The Local Negotiating Committee can support employees when they fail to reach agreement with employers. Discussion with an independent supportive colleague, mediation and trade union (British Medical Association, Hospital Consultants and Specialists Association) involvement may all be useful if disagreement continues.
Returning or not returning to work
The return to work process should be customised and supported by the employer - usually via the Clinical Director - with employee wellbeing, patient safety and a sustainable clinical workforce as key factors.
Even when community shielding is paused, some may choose or be advised not to return to work. This may be temporary or permanent. Such a decision would usually be made in consultation with the medical professionals caring for the shielding doctor and appropriate employer representatives.
We encourage doctors who have an extended delay in return to work and their departments to make active efforts to maintain professional and personal contact. This may include remote inclusion in department educational activities, formal and informal personal contact. Any temporary situation should be reviewed regularly in light of the changing situation.
Return to work basics
The environment and working practices in hospitals have changed dramatically since March 2020. All returning doctors will need a period of supported or supervised ‘acclimatisation’. This period should include time to assimilate new policies, new practices and behaviours relating to infection control and training or retraining in appropriate use of PPE.
The Academy of Medical Royal Colleges and the Royal College of Anaesthetists both provide guidance for doctors intending to return to practice after a sustained period of absence.
Further considerations
The evolving situation
National lockdowns began to be loosened across the UK in June 2020. At the same time, the first epidemic surge has receded, rates of infection in the community have decreased for several weeks and the social (physical) distancing rules are being relaxed. It has been announced in England that shielding has been relaxed and that at the end of July it will be paused so that workers who are shielding can return to work in August. To counter this, rates of community infection in the UK are an order of magnitude higher than in many other countries, the reproductive rate (R0) remains close to 1 and in some regions may be >1, and releasing lockdown is expected to increase this further. Local returns to lockdowns 8 have occurred as a result. Return to work for those working in healthcare is a particular challenge that is currently not addressed by governmental guidance.
The need for shielding may be dynamic. There is a significant risk of local or national outbreaks of increased infection (rebound activity) and, as we move into the winter months, there may be a sustained increase in infection rates, i.e. a second surge. SARSCoV-2 will likely remain a threat for many months or several years: an endemic infection. In the future, development of a vaccine may ease pressures but this, and its timeline, is far from certain. Improved knowledge of community risk and hospital staff and patient infection rates may enable a more adaptive response to shielding. The possibility of the need for sustained or episodic workplace shielding needs to be considered.
What we know about shielding doctors
The government records 2.2 million people as shielding, of whom approximately 630,000 are part of the normal workforce. The number of shielding doctors is unknown, but postgraduate training bodies are in the process of identifying numbers of shielding trainees in several counties in the UK. Shielding is not mandatory, and some doctors at equally high risk as those who are shielding may have elected not to do so.
A survey on social media of shielding doctors in Spring 2020 found similar numbers of consultant and trainees shielding. Ninety-one percent were shielding due to their own health condition and 9% ‘shielding by proxy’.
Full pay should be received while shielding, and for most is not a significant financial burden, although loss of income from on call supplements may be a concern for some. The financial burden to those who are shielding may change significantly if rules are changed and when community shielding is paused.
Psychological aspects of shielding
Government figures state that more than one third of shielding individuals reported a deterioration in their mental health as a result, with males and those aged <60 yrs more likely to be affected. The social media survey of shielding doctors identified disruption to professional lives and concerns about career progression, pay, employment and training. Shielding affected doctors’ relationships at home, alcohol use, and led to changes in behaviours and a heightened focus on their own health. Feelings of guilt, anxiety, isolation and frustration were prominent.
Psychological wellbeing is of paramount importance to working safely as a doctor, and while all aspects of this pandemic have impacted individual wellbeing, it is likely that shielding poses its own psychological stresses. Shielding involves doctors being labelled as ‘extremely clinically vulnerable’, physically removing themselves from the workplace to stay at home, inside, without contact with the outside world for many weeks. Conversely, a return to work exposes the doctor to an environment of dramatically increased exposure and risk.
Work is a hugely important part of many people’s lives. Doctors working in anaesthesia and critical care units are generally high achieving and highly motivated. Work provides a sense of purpose, a structure, friendship, camaraderie and likely a source of personal satisfaction, and contributes to a sense of self-worth. For those who are shielding these may all be lost overnight. Shielding leads to physical and professional isolation. This may be mitigated if the shielding doctor is able to continue performing useful roles from home and conversely will likely be exacerbated if this is not feasible or personal contact with the department is lost.
Psychological challenges of a return to work
For doctors who decide to return to work this will be a challenging time, and the resulting impacts should not be underestimated. Personal priorities may have changed, and return to work will involve adapting to the new ‘COVID-19 environment’. Some people will feel lonely, forgotten, guilty or bored. Most will be anxious about returning to work, with concern about their safety combined with the challenge of managing the constantly changing guidelines. Many of those who have remained at work have experienced significant psychological stress and moral injury. Some will have cared for other healthcare professionals and colleagues who have been critically ill or have died. Some may have post-traumatic stress symptoms (PTSS) and psychiatric caseness, a marker of major depression. The Society of Occupational Health Medicine has partnered with other organisations to produce two toolkits for returning to work after COVID-19 lockdown and for sustaining work-relevant mental health after COVID-19. Both are likely to be of value for leaders and individuals.
It is important that normal responses to stress are not over-medicalised, and an important factor in staying psychologically healthy is receiving and providing peer support. Independent, external support may be helpful, and the Association of Anaesthetists has a network of trained mentors. Trainees should have access to professional support units and coaching through Schools of Anaesthesia or postgraduate training bodies. Some of those returning to work might consider training in psychological first aid in order to be better able to practise self-care and recognise more severe or incapacitating mental health problems in colleagues. The Association of Anaesthetists and Royal Medical Benevolent Fund have produced online guidance for anaesthetists wellbeing in the COVID crisis and the Intensive Care Society has produced COVID specific wellbeing resources.
Return to work may also require adapting to new and unfamiliar roles or locations. It is a time to focus on retained and transferrable skills, as confidence will likely be a greater challenge to many than competence. Even experienced doctors may feel immense pressure to perform and may experience imposter syndrome or lack of confidence. Early and simple support is likely to be very beneficial. Some suggested principles are:
Examine the senior modules in the relevant syllabus relating to your new role, decide which you have maintained and identify any weaknesses. The focus is likely to be on confidence;
Establish a formal support structure. Some may benefit from attending a local or national return to work course if available;
Identify a specific colleague (buddy) who respects you and whom you respect. Be prepared to discuss changing if the relationship is not working;
Choose a small number of supportive colleagues to work with regularly during the return to work program;
Choose a longer time frame for support than you think you need. Shorten it if you need to later on;
Consider a reflective journal. This can help prevent you ruminating by allowing you to ‘dump’ your thoughts in it, for instance after a bad day. The journal will help you to see your experiences in perspective and, over time, the progress you are making.
Understanding risk
Risk is described complex subject deserving of its own document: some summary comments are made here.
Relative risk describes the extent to which one individual or group is at risk compared to a comparator individual or group, while absolute risk describes a specific numerical risk of an event, for instance as a percentage, proportion or fraction. Absolute risk is a more relevant measure of risk but is harder to determine. As risk rises, the increase in absolute risk that someone of higher relative risk is exposed to is amplified compared to someone of lower risk. Risk from COVID-19 involves either those who are more likely to get infected or those whose illness is likely to be more severe and therefore whose outcomes may be worse. As healthcare workers are generally younger than the general population, outcomes might be expected to be better than for those in unselected cohorts.
Risk of infection
Transmission of infection is likely to be affected more by exposure and behaviour than predisposing factors, and is related to the proximity and duration of exposure to infected individuals. Contact indoors is of much greater risk than outdoors, and exposure in a household is likely the highest risk. Shared transport, e.g. public transport, is also high risk. Hospitals are high risk because of exposure to infected patients, involvement in specific procedures, exposure to infected staff and difficulty in maintaining physical distance when delivering healthcare. The likelihood of exposure to infected patients depends on community transmission rates, admission policies, ability to segregate infected from noninfected patients and work patterns. Risk is increased during periods of high or rising community transmission (R0 >1). The risk of staff-staff transmission is a significant problem in hospitals and rates of hospital staff infection are several-fold higher than in the community.
At the time of writing, across the UK population, approximately 1 in 1 700 of members of the public is infected with SARS-CoV-2 and 5 - 7% have antibodies indicating previous infection, with the highest regional rates being approximately 15%. Conversely, in hospitals, approximately 1 in 60 patient-facing members of staff are infected with SARS-CoV-2 and reports of antibody positivity range from 6 - 45%.
Risk of serious and fatal illness
The most important factors, in descending order of importance are
Age: this is the dominant determinant of outcome. Risk of death increases by about 10-12% per year, doubling every 5 - 6 years and increasing 10-fold over 20 years. The effect is multifactorial but as an isolated risk factor, risk of death from COVID-19 increases three-fold from age 40 - 49 to age 50 - 59 and 6-fold to age 60 - 69.
Risk of death for men is twice that of women both among hospitalised patients and in the general population. For men and women with equivalent disease severity, there is little difference in ICU mortality.
Ethnicity: there is clear evidence of an excess mortality in the non-white UK population, and this has been highlighted in several reports. Causes are multifactorial. Sociological factors include increased exposure to urban dwelling, social deprivation, overcrowded and multigenerational housing, occupation in key worker and public-facing and 11 patient-facing roles, and reliance on public transport. Increased rates of hypertension, cardiac disease, diabetes, chronic kidney disease and obesity contribute in some populations. Genetic predisposition and relative insufficiency of Vitamin D are proposed but unconfirmed causes. A recent NICE review reported insufficient evidence to support a role for Vitamin D in preventing COVID-19, including in susceptible groups but supported current advice on daily Vitamin D supplementation in people of African, African-Caribbean or South Asian family origin. Risk varies amongst different non-white ethnicities. Early ICNARC reports highlighted disproportionately high rates of non-white, particularly black, patients in ICU. An ISARIC study highlighted an increased risk of ICU admission in all non-white ethnicities and a 20% increased mortality among patients of South Asian ethnicity, with diabetes as a contributory factor. The OPENSAFELY study reported an approximately 60-70% increase in mortality from COVID-19 across the UK population in people of non-white ethnicity.
Comorbidities: risk is increased in patients with comorbidities. Risk estimates vary even for common conditions. For uncommon or rare conditions, data are sparse and risk estimates prone to uncertainty or fluctuating estimates. The impact of deconditioning or frailty from chronic health conditions has not been widely presented. Individual comorbidities associated with increased risk of harm are chronic cardiac disease, diabetes, chronic non-asthma respiratory disease, asthma requiring oral steroids, significant obesity (body mass index >35 kg.m-2), current or previous malignancy, immunosuppression, rheumatological conditions and chronic renal or liver disease.
Risk specific to healthcare workers and specifically to anaesthetists and doctors working in critical care
The frequencies with which UK healthcare workers are admitted to hospital or ICU with COVID-19 are not reported. There is no compelling evidence that working as a healthcare worker increases the severity of COVID-19, but there is a paucity of data. Amongst healthcare workers there is no clear evidence that anaesthetists and doctors working critical care are at increased risk of infection. What evidence there is suggests decreased risk of harm.
A review by the Office for National Statistics stated that healthcare workers were not at increased risk of death. In a cohort of 166 healthcare workers who died with COVID-19 there were no anaesthetists or doctors working in critical care, but a disproportionate number of deaths were among staff members of non-white ethnicity: 64% were non-white, compared with 21% of the NHS workforce and 13% of the wider population. Amongst 31 doctors who died, 94% were non-white.
International data support the conclusion that anaesthesia and critical care medicine are not particularly high-risk specialties for infection or harm from COVID-19. It is likely that strict use of precautionary infection control measures including, but not limited to, meticulous adherence to current practices with PPE has had an important part of staff protection.
Risk calculators for healthcare workers
Smith and Spiegelhalter state the need to “communicate realistic levels of risk as they apply to different groups, not to reassure or frighten but to allow informed personal decisions in a setting of necessary uncertainty”. This is particularly important for healthcare workers as shielding is paused. Several authors have created risk calculators for healthcare workers 12
The ISARIC study links to an interactive risk tool based on its findings enabling estimation of mortality after hospital admission.
Strain et al used population disease prevalence data and risk ratios from ISARIC to estimate risk of death compared to a healthy female aged 50 and validated this using the OpenSAFELY methodology. Measures of relative risk were then adjusted and combined into low, middle and high-risk categories.
Coggon et al using OpenSAFELY study data converted increased personal relative risk into the equivalent is ’added years’- to create the ‘Covid-age’ tool
The Association of Local Authority Medical Advisors uses Covid-age to categorise into vulnerability categories and workplace adjustments.
NHS Employers use a tool that supports workplace and workforce risk assessment, but lacks quantitative assessment of personal risk.
The Welsh COVID-19 workforce risk assessment tool scores personal risk in broadly terms and allocates categories and graded responses.
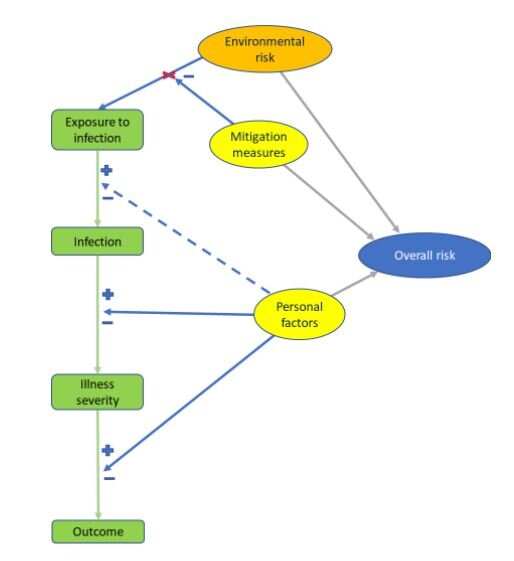
There are limitations to all these tools. First, most only use personal (mostly biological) factors to assess risk. Although intended for healthcare professionals, they do not capture the interaction between personal and work-related environmental risk or mitigation of the latter (Figure 2). There is a danger they are simply population risk tools. Several tools group risk scores to create ‘categories of risk’. However, as risk is a continuous variable, this categorisation is artificial, creating particular problems for those just below or just above a boundary. Categorisation also lends itself to definitive allocation of specific actions to specific categories. The failure to consider the dynamic impact of workplace and rolerelated risks and categorisation may make the tools rigid and unable to adapt to variations in prevalence and mitigation. This is particularly important to higher risk individuals who are most affected by dynamic changes in risk. Because of the limitations of the underlying data on which COVID-19 risk tools are based, it is likely that they are best used a guide to risk and to inform discussions rather than determine outcomes.
Figure 2
Resources
Links to useful resources of importance or in addition to those embedded in the document
TERMS AND CONDITIONS
HSE Guidance - https://www.hse.gov.uk/guidance/index.htm
HSE legal responsibilities home workers - https://www.hse.gov.uk/toolbox/workers/home.htm
NHS Employers guidance https://www.nhsemployers.org/covid19/health-safety-andwellbeing/supporting-our-most-vulnerable-people
Reasonable adjustments policy https://www.nhsemployers.org/retention-and-staffexperience/diversity-and-inclusion/policy-and-guidance/disability/reasonableadjustments-in-the-workplace
Risk assessments for staff https://www.nhsemployers.org/covid19/health-safety-andwellbeing/risk-assessments-forstaff?fbclid=IwAR3e4NfHQcHJe6aoD0JgGjVz9yeWxIsqUa43g4RUZ5-FclOyJuZthu25B0k
Staff with childcare abilities https://www.nhsemployers.org/covid19/health-safety-andwellbeing/supporting-staff-with-childcare-responsibilities
RIDDOR reporting COVID - https://www.hse.gov.uk/coronavirus/riddor/index.htm
FOR TRAINEES
Health Education England. Supported Return to Training. Sub-site https://www.hee.nhs.uk/our-work/supporting-doctors-returning-training-after-time-out and COVID-19 https://www.hee.nhs.uk/coronavirus-covid-19
Denison A, Metcalf L, Shielding and Postgraduate Training in the Scotland Deanery.pdf Scotland Deanery 28 May 2020 Iliff HA, Simpson KA, Tomlinson CR, Webb CM on behalf of Anaesthetists, Intensivists Shielding. ‘Shielded’ anaesthetists and intensivists during the COVID‐19 pandemic. https://doi.org/10.1111/anae.15153
RISK STUDIES Office for National statistics: Coronavirus (COVID-19) Infection Survey pilot https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/england14may2020
The OPENSAFELY collaborative. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. https://www.medrxiv.org/content/10.1101/2020.05.06.20092999v1
Reports from International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) at https://isaric.tghn.org/covid-19-clinical-research-resources
Docherty AB, Harrison EM, Green CA et al. Features of 20133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 2020;369:m1985 (at https://www.bmj.com/content/bmj/369/bmj.m1985.full.pdf )
Intensive Care national Audit and Research Centre reports – at https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
Speigelhalter D. What have been the fatal risk of Covid particularly to children and younger adults. https://medium.com/wintoncentre/what-have-been-the-fatal-risks-ofcovid-particularly-to-children-and-younger-adults-a5cbf7060c49
Platt L, Warwick R. Are some ethnic groups more vulnerable to COVID-19 than others?
Institute for Fiscal Studies. https://www.ifs.org.uk/inequality/chapter/are-some-ethnicgroups-more-vulnerable-to-covid-19-than-others/
Razaq A, Harrison D, Karunanithi S et al. BAME COVID-19 DEATHS – What do we know? Rapid Data & Evidence Review. Centre for Evidence Based Medicine. https://www.cebm.net/covid-19/bame-covid-19-deaths-what-do-we-know-rapid-dataevidence-review/
Public Health England. Beyond the data: Understanding the impact of COVID-19 on BAME groups. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment _data/file/892376/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf Odds ratios for risk of coronavirus-related deaths by ethnic group, England and Wales. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/dea ths/datasets/oddsratiosforriskofcoronavirusrelateddeathsbyethnicgroupenglandandwales
RISK TOOLS
Clinical guide for the management of Rheumatology patients during the coronavirus pandemic https://www.england.nhs.uk/coronavirus/wpcontent/uploads/sites/52/2020/03/clinical-guide-rheumatology-patients-v2-08-april2020.pdf
DEATHS OF HEALTHCARE WORKER, ANAESTHETIST AND INTENSIVISTS
Cook TM, Kursumovic E, Lennane S. Exclusive: deaths of NHS staff from covid-19 analysed. https://www.hsj.co.uk/exclusive-deaths-of-nhs-staff-from-covid-19- analysed/7027471.article
Cook TM, Kursumovic E, Lennane S, Kearney L, Woodman E. Younger female NHS workers may face greater risk of death from coronavirus. https://www.hsj.co.uk/coronavirus/younger-female-nhs-workers-may-face-greater-risk-ofdeath-from-coronavirus/7027560.article
Kearney L, Lennane S, Woodman E, Kursumovic E, Cook TM. At least 23 nationalities among NHS staff killed by covid. https://www.hsj.co.uk/workforce/at-least-23-nationalitiesamong-nhs-staff-killed-by-covid/7027666.article
Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID‐19: the need for robust data and analysis. First published:12 May 2020 Podcast https://topmedtalk.libsyn.com/covid-19-black-and-minority-ethnic-bame-deathrates-update-from-the-uk
PRACTICAL and PSYCHOLOGICAL SUPPORT
Simple strategies to maximise the day and maintain physical and mental wellbeing https://anaesthetists.org/Home/Resources-publications/COVID-19-guidance/Maximiseyour-day-while-shielding
Society for Occupational Medicine: returning to the workplace after the COVID-19 lockdown – toolkit https://www.som.org.uk/return-to-work/
Society for Occupational Medicine: sustaining Work-Relevant Mental Health Post COVID19 Toolkit https://www.som.org.uk/Sustaining_work_relevant_mental_health_post_COVID19_toolkit.pdf
NHS Guide Shielding and returning to work https://people.nhs.uk/guides/shielding-andreturning-to-work/
WEBINARS
Dr Sethina Watson gave a talk about the impact of shielding on anaesthetists in a recent Association webinar (time point 1:04:45 in: https://register.gotowebinar.com/recording/viewRecording/8054623469383961613/391724 0379133570566/andrewmortimore@anaesthetists.org?registrantKey=2674782344143402252 &type=ABSENTEEEMAILRECORDINGLINK
Authors
Tim Cook, Tei Sheraton, Sethina Watson, Ros Bacon, Caroline Evans, Karen Kidner, Jack Parry-Jones, Fiona Donald, Will Harrop Griffiths, Kathleen Ferguson